Diabetes is much more than just a condition characterized by elevated blood sugar. It’s a systemic problem that subtly impacts many body parts, particularly the nerves in your legs and feet. Uncontrolled blood sugar levels have the potential to harm these nerves over time, resulting in diabetic neuropathy.
Here’s why it’s concerning …
The World Health Organization estimates that 422 million people worldwide have diabetes, with 77 million of those cases occurring in India, often called the diabetes capital of the world.
Dr. Ayush Chandra, an accomplished Diabetologist in Ghaziabad, says:
“Diabetic leg and foot pain isn’t just discomfort—it’s a signal that the nerves and circulation are under strain. Many people ignore the early tingling or burning, but addressing these signs promptly can prevent serious complications like ulcers or infections. My advice is simple: never dismiss mild pain or numbness if you’re diabetic.”
But how can you tell whether the discomfort in your feet is actually linked to diabetes or something else? Let’s dig deeper into the telltale signs.
Recognizing Diabetes-Related Foot Pain
Foot pain in diabetes can sometimes be subtle at first. You might feel mild tingling, burning, or a sensation as if you’re walking on pebbles. These are often early symptoms of diabetic leg pain caused by nerve damage. Over time, this can progress to numbness, making it harder to feel cuts or blisters — which in turn increases the risk of infection.

Here are some common indicators that your foot pain may be diabetes-related:
Persistent tingling or burning: A sign of nerve irritation due to high blood sugar.
Loss of sensation: You may not feel pain, heat, or cold in your feet.
Muscle weakness: Difficulty walking or maintaining balance.
Slow-healing wounds: Even small injuries take longer to recover.
Foot deformities or skin changes: Calluses, dry skin, or ulcers may appear without you noticing.
Dr. Ayush Chandra, a highly regarded Diabetic Foot Specialist in Ghaziabad, explains:
“Recognizing these early symptoms is crucial. Many patients come to us when pain has already turned into numbness. At that stage, injuries can go unnoticed and escalate quickly. The sooner you identify nerve-related pain, the better your chances of preventing diabetic foot ulcers.”
Feeling tingling or numbness in your feet? Seek timely guidance from a Diabetic Foot Specialist to understand your symptoms and protect your mobility.
Now that you know the signs, it’s important to understand why this happens in the first place.
Common Triggers Behind Diabetic Leg and Foot Pain
The primary reason behind diabetic foot pain is nerve damage (diabetic neuropathy), but several factors can worsen the condition. Understanding these causes helps in managing the problem effectively.
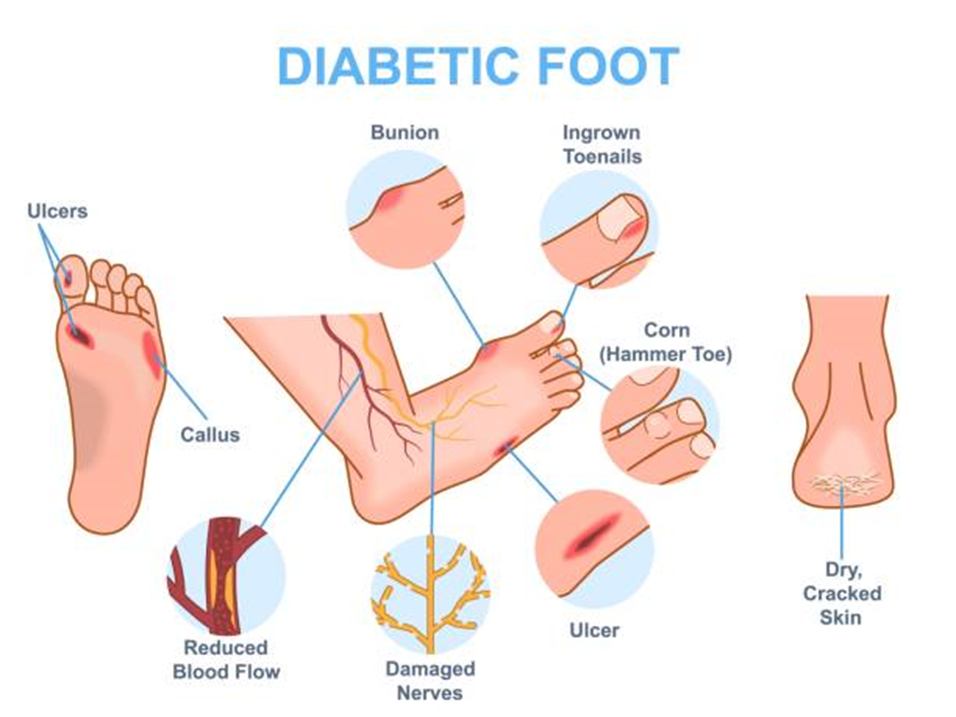
Uncontrolled blood sugar: Constantly high glucose levels damage nerve fibers and blood vessels supplying the feet.
Poor circulation: Diabetes narrows and hardens blood vessels, reducing oxygen supply to nerves and tissues.
Inflammation of nerves: Chronic inflammation can increase sensitivity and pain.
Lifestyle factors: Smoking, obesity, and lack of physical activity accelerate nerve damage.
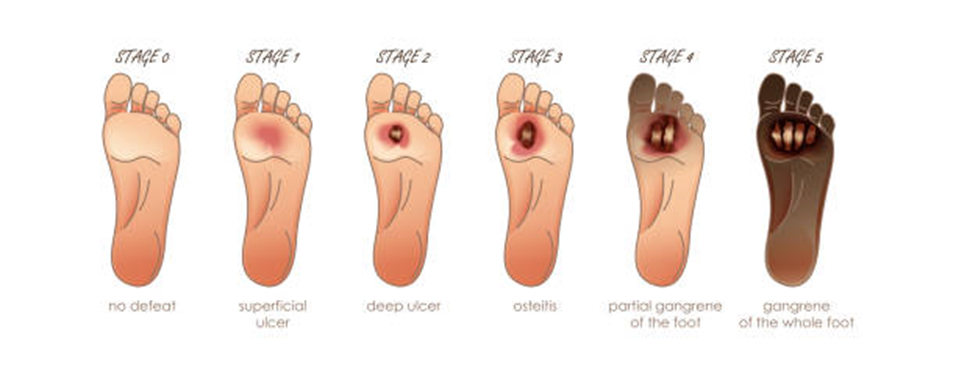
Infections and ulcers: Minor wounds can develop into diabetic foot ulcers if ignored.
Dr. Ayush Chandra, an insightful Diabetologist in Ghaziabad, adds:
“The interplay between nerve damage and poor circulation makes diabetic leg pain complex. It’s not only about nerves—blood flow, footwear, and daily habits all contribute. By controlling blood sugar and following proper foot care, patients can significantly delay or prevent neuropathy.”
Knowing the cause gives clarity—but what can you do about it? Let’s explore practical steps to manage this pain effectively.
Managing Diabetic Foot Pain
Managing diabetic foot pain involves a combination of medical treatment, lifestyle adjustments, and daily self-care. Here’s how you can take control:

Maintain blood sugar levels: Regular monitoring and medication adherence are the foundation.
Foot care routine: Wash feet daily, dry them well, and check for blisters or cuts.
Wear proper footwear: Use shoes that support the arch and reduce pressure points.
Exercise regularly: Activities like walking or swimming improve circulation.
Pain relief therapies: Depending on severity, doctors may prescribe medications for pain relief for diabetic foot pain, such as nerve-calming drugs or topical ointments.
Nutritional support: Diets rich in B-vitamins and antioxidants help maintain nerve health.
Dr. Ayush Chandra, a dedicated Diabetic Foot Specialist in Ghaziabad, shares:
“Foot pain management is most effective when approached holistically. Alongside medication, I recommend patients focus on movement, hydration, and nutrition. Each small step towards better self-care reduces complications dramatically.”
Struggling with diabetic foot discomfort? Consult a Diabetic Foot Specialist to receive a personalized plan for managing pain and preventing long-term damage.
Even with the best care, sometimes pain might indicate something more serious. So, when should you worry?
When Foot Pain Demands Immediate Attention
Dr. Ayush Chandra, a reputed Diabetologist in Ghaziabad, emphasizes:
“Ignoring warning signs can turn a manageable issue into a serious complication. If you notice ulcers or swelling, don’t self-medicate. Proper assessment can prevent infections from spreading or requiring surgical intervention.”
Understanding severity helps you act fast—but long-term protection lies in awareness and consistency.
Conclusion
Diabetic leg and foot pain is more than a symptom—it’s a reminder to take charge of your health. Managing blood sugar, maintaining foot hygiene, and seeking timely help can make all the difference. Early detection not only prevents discomfort but also safeguards against irreversible nerve damage
Noticing unusual sensations in your feet? Consult a Diabetologist to get evaluated and receive expert guidance on preventing diabetic foot complications.
Before we wrap up, let’s address some common questions that patients often ask about diabetic foot pain and care.
FAQs
- Can diabetic foot pain be reversed?
Complete reversal is rare, but improvement is possible. When blood sugar levels stay within a healthy range and daily care becomes consistent, many people notice less pain and better nerve response. The idea is to slow the damage down and giving your nerves a chance to heal where they can.
- What is the best pain relief for diabetic foot pain?
Pain relief depends on the cause and severity. When used regularly, people find relief through various options including:
- Medications for nerve pain
- Topical creams
- Simple physical therapies recommended by your doctor
- Supportive shoes
- How can I prevent foot ulcers from developing?
Ghaziabad’s trusted Diabetic Foot Specialist, Dr. Ayush Chandra, advises:
“Start by treating your feet like they matter—because they do. Inspect your feet daily, keep them clean and dry, wear well-fitting shoes, and never walk barefoot. Regular visits to your Diabetologist can help detect early signs of pressure or injury.”
- Is diabetic neuropathy reversible?
Early-stage diabetic neuropathy may improve with strict glucose control and lifestyle changes, but advanced nerve damage is usually permanent. However, pain can be managed effectively with medical support.
- What’s the best time to visit a doctor for diabetic foot pain?
At the very first sign of tingling, numbness, or slow-healing wounds. Early consultation ensures timely intervention and prevents severe complications like diabetic foot ulcers.
Disclaimer: This article is for educational purposes and should not be considered a substitute for professional medical advice. Always speak with a healthcare provider about your specific concerns.


