Diabetic wounds are a serious concern, often leading to prolonged healing and increased risks of infection. Vacuum-Assisted Closure (VAC) Therapy, also known as Negative Pressure Wound Therapy, is a revolutionary treatment promoting tissue regeneration and healing. Globally, VAC Therapy has been extensively used, with studies showing it can reduce wound healing time by 50% compared to conventional methods.
Dr. Ayush Chandra, Founder and Director of Nivaran Health in Ghaziabad, explains:
“Chronic wounds impact not only a patient’s health but also their quality of life, leading to pain, infections, and even amputations in severe cases. Fortunately, advancements like VAC Therapy for wound healing have transformed patient outcomes, making recovery faster and safer.”
This page provides in-depth insights into the role, benefits, procedure, and success rates of VAC Therapy for Diabetic Wounds.
Role of VAC Therapy in Diabetic Wounds
Patients suffering from diabetic wounds can significantly benefit from VAC Therapy for faster recovery. It can help overcome the challenges of slow healing caused by poor circulation and infection risks.
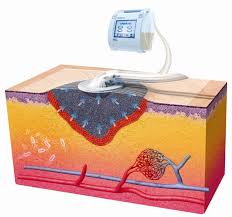
It works by applying controlled suction to the wound, effectively reducing swelling, removing excess fluids, and promoting tissue regeneration. This tissue regeneration therapy creates an ideal environment for healing, prevents infections, and accelerates wound closure.
Are you struggling with a slow-healing diabetic? Consult a specialist today to explore how VAC Therapy can accelerate your recovery.
VAC Therapy offers multiple advantages, but understanding the benefits and risks can help patients make informed decisions.
Benefits:
- Faster Healing: VAC therapy’s controlled suction helps remove excess fluid from the wound bed, creating an optimal environment for new tissue growth and accelerating the healing process.
- Reduced Edema: By drawing out excess fluid, VAC therapy effectively reduces swelling around the wound, improving tissue perfusion and promoting healing.
- Stimulation of Granulation Tissue: The negative pressure applied by the VAC device encourages the formation of granulation tissue, which is crucial for wound closure.
- Decreased Bacterial Load: The vacuum effect can help remove debris and bacteria from the wound, potentially reducing the risk of infection.
- Improved Blood Flow: VAC therapy enhances circulation to the wound site, ensuring an adequate supply of oxygen and nutrients to promote faster healing.
- Management of Large, Exudating Wounds: This therapy is particularly beneficial for large, draining diabetic wounds, as it effectively controls drainage and maintains a clean wound bed, reducing the risk of infection.
- Potential for Limb Preservation: By facilitating the healing of diabetic foot ulcers, VAC therapy can significantly reduce the chances of amputation in severe cases, offering patients a better quality of life.
- Skin Irritation: Some patients may experience redness or irritation around the treated area.
- Bleeding: If the wound involves exposed blood vessels, there is a potential risk of minor bleeding.
- Device Malfunction: The therapy requires continuous suction, and improper usage may lead to delayed healing.
- Cost Factor: As an advanced therapy, it may be costlier than traditional treatments.
Eligible Candidates
Patients who may benefit from VAC Therapy for wound healing include:
- Those with chronic, non-healing diabetic wounds.
- Individuals with post-surgical wounds at risk of infection.
- Patients with pressure ulcers or venous ulcers.
- Those with traumatic wounds requiring controlled healing.
Dr. Ayush Chandra, an expert in diabetes and obesity treatment, states:
“The right candidates for VAC Therapy are those struggling with persistent wounds despite conventional treatments. A proper evaluation can determine if this advanced wound care solution is the best approach for a patient’s recovery.”
Preparing for VAC Therapy in Diabetic Wounds
Before you begin treatment, there are essential steps to ensure the best results. Here’s what you need to know.
Medical Assessment: A thorough evaluation to assess the wound’s severity.
Blood Sugar Control: Maintaining stable glucose levels helps heal wounds faster.
Wound Care: The area must be clean of debris to prevent infection.
Dressing Selection: The appropriate foam dressing is chosen based on wound size and depth.
Procedure
Foam Dressing Placement: A specialized porous material is carefully applied to cover the affected area. This allows even distribution of negative pressure while protecting the wound from external contaminants.
Sealing the Dressing: A transparent, adhesive film is placed over the foam dressing. This airtight seal prevents bacteria and external moisture from entering the wound while helping to maintain the necessary pressure for tissue regeneration.
Vacuum Application: A controlled suction device, connected through a small tube, is activated to maintain negative pressure across the wound site. This helps remove excess fluids, reduces swelling, improves blood circulation, and accelerates new tissue formation for more efficient healing.
Monitoring: The wound is monitored regularly to assess progress and prevent complications.
Are you curious about healing wounds faster with VAC therapy? Consult a specialist today to explore your options.
What happens after the procedure? Let’s walk through the recovery process and key post-care tips.
Side Effects & Post-op Care Guidelines:
- Ensure the dressing remains sealed and intact. If it becomes loose or leaks, contact your healthcare provider immediately.
- Mild discomfort is common; pain relievers may be prescribed if necessary. Avoid over-the-counter medications without medical advice.
- Redness, warmth, foul odor, or unusual discharge should be reported to a doctor promptly.
- Keep the surrounding skin clean and dry to prevent irritation or infection. Avoid unnecessary handling of the dressing.
- Lifestyle modifications including a balanced diet rich in protein, vitamins, and minerals supports faster tissue regeneration.
- Avoid excessive movement or pressure on the wound area to promote optimal healing.
- Regular check-ups allow the doctor to assess progress and make necessary adjustments to the treatment.
Recovery Timeline:
First Few Days: Reduction in swelling and fluid drainage, with the wound beginning to adapt to negative pressure therapy.
1-2 Weeks: Noticeable improvement in wound size, reduced exudate, and formation of healthy granulation tissue.
4-6 Weeks: Significant healing with proper tissue formation, improved skin integrity, and reduced risk of complications.
Success Rates
VAC Therapy has transformed diabetic wound care, demonstrating high success rates globally. Studies indicate that VAC Therapy for diabetic wounds has a 70-80% success rate in preventing infections and promoting complete healing. Globally, VAC Therapy has shown a 60-70% success rate in treating complex diabetic wounds, making it one of the most advanced wound care treatments available today.
Dr. Ayush Chandra, a proficient diabetologist and liver specialist in Ghaziabad, shares:
“The integration of VAC Therapy in diabetic wound care has drastically improved outcomes, allowing patients to recover with minimal complications. Ongoing research continues to refine these techniques, making treatments even more effective.”
Conclusion
Chronic wounds can be distressing and significantly impact daily life. Fortunately, with medical advancements like VAC Therapy for diabetic wounds, patients have a much higher chance of healing effectively.
Diabetes expert Dr. Ayush Chandra emphasizes:
“Wound healing in diabetic patients requires specialized care. With cutting-edge therapies like Negative Pressure Wound Therapy, we can ensure faster recovery and a better quality of life. Continued research aims to enhance these treatments for even greater success.”
Struggling with a slow-healing diabetic wound? Reach out to a qualified diabetologist and explore advanced wound care treatments to improve your healing journey.
Let’s address some of the most common concerns about VAC Therapy.
FAQ
How does VAC Therapy differ from traditional wound care?
VAC Therapy creates negative pressure to remove fluids and stimulate healing, whereas traditional wound care relies on dressings and antibiotics.
Can VAC Therapy be used for all diabetic wounds?
Not all wounds are suitable. A doctor will assess factors such as size, infection risk, and tissue health before recommending treatment.
How long does VAC Therapy take to show results?
Most patients see improvement within 1-2 weeks, with significant healing occurring within 4-6 weeks.
Does VAC Therapy require hospitalization?
In many cases, it can be done on an outpatient basis, but complex wounds may require short hospital stays for monitoring.
Is VAC Therapy painful?
Mild discomfort may occur, but it is generally well-tolerated. You can discuss pain management strategies with your doctor.
Reference Links:
https://www.pcdsociety.org/resources/details/vacuum-assisted-closure-therapy-for-the-diabetic-foot
Disclaimer: The information shared in this content is for educational purposes only and not for promotional use.